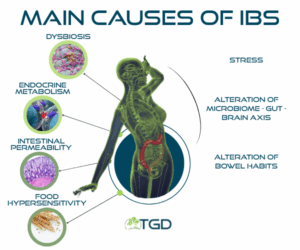
Irritable bowel syndrome (also known as irritable colon, spastic colitis, or IBS) is a common and often hard-to-diagnose functional gastrointestinal disorder. It is considered a chronic or recurrent condition in which normal gastrointestinal function is altered, but no structural disease can be demonstrated. IBS affects approximately 10% of the population, primarily women aged 20 to 50. Main symptoms include abdominal pain, bloating, diarrhea, and/or constipation.
How is IBS diagnosed?
Despite its complexity, IBS diagnosis is based on reported symptoms and follows the ROME IV diagnostic criteria. There are five recognized subtypes of IBS:
-
IBS-D: predominantly diarrhea;
-
IBS-C: predominantly constipation;
-
IBS-M: mixed bowel habits;
-
IBS-U: unclassified;
-
Post-infectious IBS: develops after infectious gastroenteritis caused by bacteria, viruses, or parasites.
Key features of Irritable Bowel Syndrome
Five key elements are typically considered during diagnosis:
-
Altered gut motility: either faster or slower intestinal transit
-
Visceral hypersensitivity: increased perception of intestinal pain
-
Abdominal bloating: present in about half of patients
-
Intestinal inflammation
-
Gut dysbiosis
All of these aspects relate to the gut-brain axis, now more accurately defined as the brain-gut-microbiota axis. A complex and vital communication exists between the gut microbiota, enteric nervous system, and central nervous system. Through neural and hormonal signals, these systems collaborate to regulate normal digestive functions. When this balance is disrupted, functional gastrointestinal disorders can occur.
A Healthy Gut Microbiota
The intestinal microbiota plays a complex and beneficial role in human health. It helps metabolize various compounds, produce micronutrients, and stimulate the immune system. Although bacteria colonize different regions of the GI tract, most of them reside in the colon, particularly Bacteroidetes and Firmicutes phyla. The composition of the microbiota is strongly influenced by diet and can be analyzed to determine a person’s enterotype.
Dysbiosis and IBS
Dysbiosis refers to an imbalance in the composition and function of the gut microbiota.
Variations in microbial populations can contribute to IBS development and progression by inducing inflammation and local or systemic immune responses. These alterations are particularly evident in IBS-D (diarrhea-predominant), but reduced microbial diversity is considered a hallmark across all IBS types.
A specific type of dysbiosis, Small Intestinal Bacterial Overgrowth (SIBO), is associated with IBS symptoms. Studies show symptom improvement in IBS patients following SIBO treatment.
How is IBS treated?
For mild to moderate symptoms, dietary and behavioral interventions are the first choice. In more severe or persistent cases, pharmacological treatment is recommended.
Are there specific diets for IBS?
Basically, the recommended dietary modifications include a high-fiber diet and the FODMAP diet. The latter, in particular, is low in Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols, from which the acronym is derived. The low-FODMAP diet reduces all short-chain carbohydrates. These compounds have limited absorption in the small intestine and tend to be fermented by colonic bacteria, leading to the production of bothersome gas. However, since it is a very restrictive diet, it is difficult to follow over long periods.
The high-fiber diet is primarily designed to benefit patients with IBS-C. However, as shown by most related studies, fiber does not have significant effectiveness in treating IBS.
Other types of diets have also been attempted, which aim to exclude foods that promote intestinal gas production (e.g., beans, onions, cabbage, Brussels sprouts, celery, carrots, bananas, apricots, prunes, artichokes), as well as alcohol and caffeine. However, these diets seem to provide relief only in a limited number of patients.
Physical Activity
Moderate physical activity, 3–5 times per week, has been shown to improve symptoms in some patients. Given the impact of stress and anxiety on IBS, hypnotherapy and cognitive behavioral therapy (CBT) have also been explored. However, these interventions show limited and inconsistent long-term benefit.
Pharmacological Treatments
There are various medications that can be used to manage the symptoms of irritable bowel syndrome (IBS). Some examples include laxatives for constipation, antidiarrheals for diarrhea, antispasmodics for abdominal pain, and rifaximin for abdominal bloating. Since IBS is characterized by a wide range of symptoms with varying frequency and intensity, treatment should be personalized and adjusted over time.
Please note: medications should always be taken under medical advice and/or prescription!
Dietary Supplements
The most commonly used supplements for IBS are based on peppermint essential oil (Mentha x piperita). Studies show it can reduce intestinal motility and relieve pain and bloating.
Peppermint oil acts as a spasmolytic throughout the GI tract. However, it should be avoided in patients with hiatal hernia or gastroesophageal reflux disease, as it may relax the lower esophageal sphincter and worsen symptoms.
Probiotics
Probiotics are not currently recommended for IBS. Although modulating the microbiota appears promising, clinical trials have produced conflicting results regarding strain selection, dosage, treatment duration, and efficacy. Commonly used species include Lactobacillus, Bifidobacterium, Streptococcus, and Saccharomyces cerevisiae. However, optimal formulations remain undefined.
Oral probiotics also struggle to colonize the gut effectively due to barriers across the digestive tract. Most are eventually eliminated in the stool.
Postbiotics
Postbiotics are bacterial derivatives that modulate gut microbiota composition and metabolism, interacting with the immune system. Proposed for use in chronic inflammation and functional GI disorders, clinical trials have shown promising results in IBS patients.
Eubiotics
Eubiotics are positive modulators of the gut microbiota. Several natural substances, including certain essential oils, have the ability to positively influence the intestinal microbiota. Essential oils with this type of demonstrated in vitro activity must, however, be made non-absorbable in the small intestine in order to reach the colon, where the majority of the human gut microbiota resides.
One noteworthy essential oil in this regard is Palmarosa oil (Cymbopogon martinii). There is extensive scientific literature on the potential of geraniol, one of its major components. Geraniol has antimicrobial, antioxidant, and anti-inflammatory properties. Based on preclinical studies (in animal models of colitis) and a clinical study conducted by our research group, the effects of this oil—absorbed onto ginger powder to ensure it reaches the colon—were evaluated with excellent results. Supplementing the diet with Palmarosa oil absorbed onto ginger fiber reduced inflammation, counteracted dysbiosis, and alleviated IBS symptoms. Learn more about our ingredient BIOintestil®.
Conclusions
In conclusion, IBS is a functional intestinal disorder that is widespread and difficult to diagnose. The health and functionality of the gut microbiota are increasingly being recognized as central to its pathogenesis. Indeed, bacterial metabolism is closely linked to gut function and affects both the enteric and central nervous systems. It is no coincidence that the well-known “gut–brain axis” now includes the microbiota as a key component. Dysbiosis can severely affect intestinal health and is almost always present in IBS. Various therapeutic approaches exist for symptom management, ranging from dietary strategies to pharmacological treatments and supplementation with natural compounds. Among these, certain essential oils and their components stand out for their beneficial influence on gut microbiota composition.
